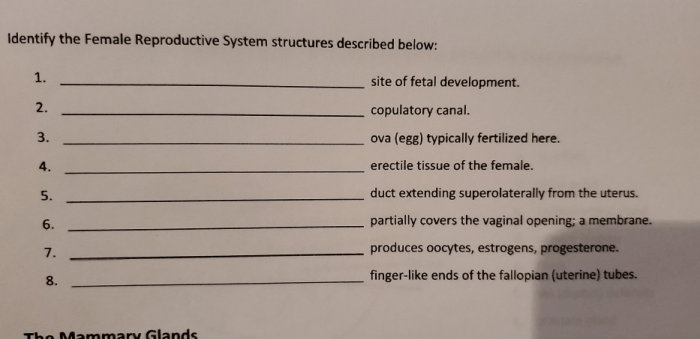
The duct extending superolaterally from the uterus, a crucial anatomical structure, plays a significant role in female reproductive physiology and pathology. This comprehensive overview delves into the intricacies of this duct, encompassing its anatomical course, histological features, clinical significance, embryological development, histopathological findings, and treatment options.
The duct’s anatomical location, variations, and anomalies are meticulously described, providing a foundation for understanding its clinical implications. Diagnostic techniques and differential diagnoses related to duct disorders are thoroughly examined, highlighting the importance of accurate evaluation.
Anatomical Overview
The duct extending superolaterally from the uterus, also known as the paramesonephric duct or Müllerian duct, is a paired structure present in female embryos. These ducts play a crucial role in the development of the female reproductive system.
Each paramesonephric duct originates from the coelomic epithelium near the mesonephric ridge and extends caudally, lying medial to the mesonephric duct. As it descends, it fuses with its contralateral counterpart to form the uterovaginal primordium, which subsequently gives rise to the uterus, cervix, fallopian tubes, and the upper part of the vagina.
Structure and Histological Features
The paramesonephric duct is a thin, tubular structure lined by a single layer of cuboidal or columnar epithelium. The epithelium is supported by a thin layer of connective tissue, which contains smooth muscle cells and fibroblasts.
Variations and Anomalies
- Uterine duplication: Occurs when the paramesonephric ducts fail to fuse properly, resulting in the formation of a double uterus.
- Unicornuate uterus: Develops when one of the paramesonephric ducts fails to develop, leading to a single, horn-shaped uterus.
- Bicornuate uterus: Arises from incomplete fusion of the paramesonephric ducts, resulting in a uterus with two distinct horns.
Clinical Significance
Abnormalities of the paramesonephric ducts can have significant clinical implications, affecting female reproductive health and fertility.
Diagnostic Implications
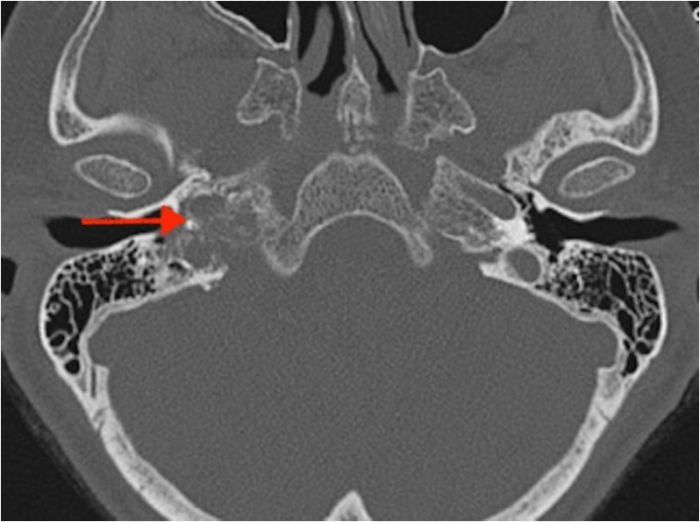
- Ultrasound: Can visualize the uterus and fallopian tubes, helping to identify structural abnormalities such as uterine duplication or unicornuate uterus.
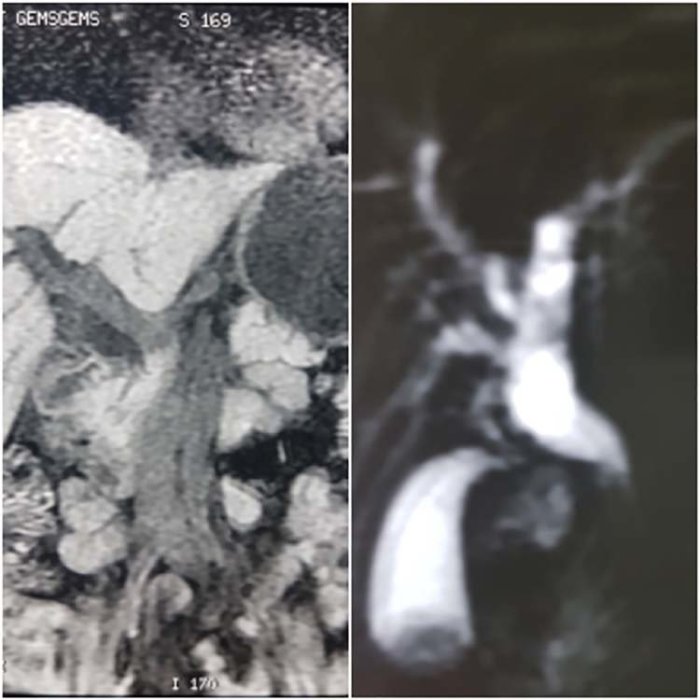
- Magnetic resonance imaging (MRI): Provides detailed images of the female reproductive organs, allowing for the evaluation of complex anomalies and their relationship to surrounding structures.
- Hysterosalpingography: Involves injecting a contrast agent into the uterus and fallopian tubes to assess their patency and identify any obstructions or abnormalities.
Clinical Presentations and Differential Diagnoses
- Infertility: Uterine anomalies can hinder the implantation or development of an embryo, leading to infertility.
- Menstrual irregularities: Abnormal uterine structures can affect menstrual flow, causing heavy or irregular periods.
- Pelvic pain: Uterine anomalies can cause pain during intercourse or menstruation due to abnormal positioning or structural issues.
Embryological Development: Duct Extending Superolaterally From The Uterus
The paramesonephric ducts originate from the intermediate mesoderm during embryonic development. Their formation is influenced by a complex interplay of molecular and genetic factors.
Molecular and Genetic Factors
- Wnt4: A signaling molecule that promotes the development of the paramesonephric ducts by inhibiting the formation of the mesonephric ducts.
- Lhx1: A transcription factor that regulates the expression of genes involved in the differentiation and maintenance of the paramesonephric ducts.
- Emx2: Another transcription factor that plays a role in the development and patterning of the paramesonephric ducts.
Significance for Clinical Practice
Understanding the embryological development of the paramesonephric ducts is crucial for clinical practice as it provides insights into the potential causes of congenital anomalies and aids in the diagnosis and management of reproductive disorders.
Histopathological Findings
Histopathological examination of tissue samples from the paramesonephric ducts can provide valuable information for diagnosing and characterizing duct disorders.
Key Histopathological Features
| Feature | Description |
|---|---|
| Epithelium | Single layer of cuboidal or columnar cells |
| Stroma | Thin layer of connective tissue containing smooth muscle cells and fibroblasts |
| Glands | May be present within the stroma, lined by cuboidal or columnar epithelium |
| Cysts | May form due to dilatation of the glands or ducts |
Diagnostic Criteria and Differential Diagnoses, Duct extending superolaterally from the uterus
The histopathological findings in paramesonephric duct disorders can help differentiate them from other conditions with similar clinical presentations, such as endometriosis or pelvic inflammatory disease.
Treatment Options
The treatment approach for paramesonephric duct disorders depends on the specific anomaly, its severity, and the patient’s individual circumstances.
Conservative Management
- Observation: For minor anomalies that do not cause significant symptoms or affect fertility.
- Hormonal therapy: To regulate menstrual cycles and manage pain associated with uterine anomalies.
Surgical Intervention
- Hysteroscopic metroplasty: A minimally invasive procedure used to correct uterine septum or other intrauterine abnormalities.
- Laparoscopic surgery: To address anomalies involving the fallopian tubes or ovaries, such as tubal ligation or ovarian cystectomy.
- Open surgery: May be necessary for complex anomalies or when minimally invasive techniques are not feasible.
Medical Therapies
- Antibiotics: To treat infections associated with paramesonephric duct anomalies.
- Pain relievers: To manage pain and discomfort caused by uterine anomalies.
Multidisciplinary Care
The management of paramesonephric duct disorders often requires a multidisciplinary approach involving gynecologists, reproductive endocrinologists, and surgeons. This collaborative approach ensures comprehensive care and optimal outcomes for patients.
FAQ Corner
What is the clinical significance of duct abnormalities?
Duct abnormalities can manifest in various clinical presentations, including infertility, pelvic pain, and abnormal uterine bleeding. Accurate diagnosis is crucial for appropriate management.
How do imaging techniques aid in evaluating duct pathology?
Imaging techniques such as transvaginal ultrasound, hysterosalpingography, and magnetic resonance imaging (MRI) provide valuable insights into duct anatomy and pathology, aiding in diagnosis and treatment planning.
What are the key histopathological features of duct disorders?
Histopathological examination reveals characteristic features such as epithelial hyperplasia, stromal fibrosis, and inflammatory cell infiltration, which aid in diagnosing and differentiating duct disorders.